The Data Quality Illusion: Why Aggregated EHR Feeds Often Fail
- February 12, 2026
- Posted in Lab Testing Insights
- Posted in Commercial Launch Excellence
- Posted in Rare Disease
- Posted in Oncology
- Posted in Field Force Effectiveness
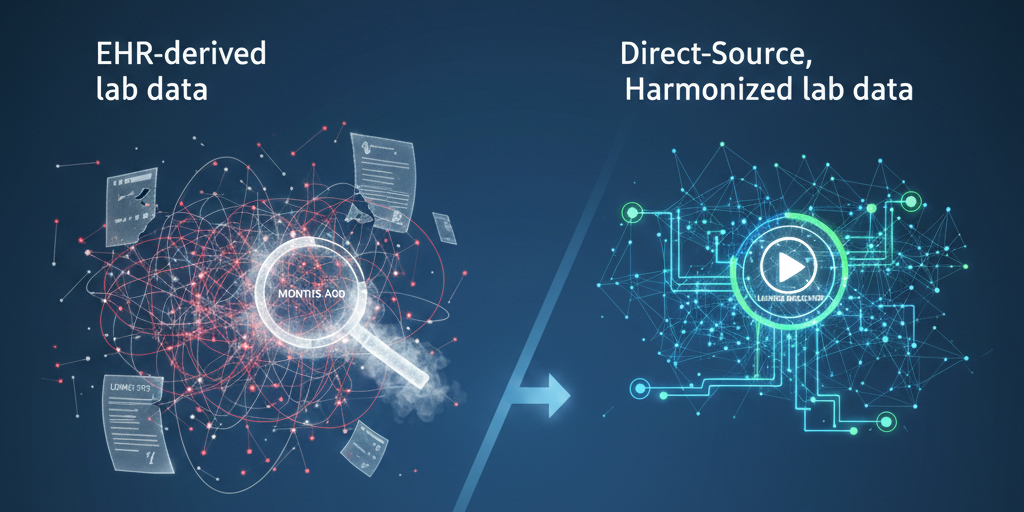
In the life sciences industry, "lab data" is often treated as a commodity. The assumption is that a lab result is a lab result, regardless of where it comes from. However, as commercial teams pivot toward rare and complex diseases, a critical structural flaw is emerging: the vast difference between EHR-derived lab data and Direct-Source, Harmonized lab data.
While aggregated EHR feeds are widely available and often appear cost-effective, they are functionally distinct from direct-source data. Understanding this distinction is often the difference between a successful precision medicine launch and a missed market opportunity.
The Standardization Gap: "Projectware" vs. Analytics-Ready
The primary challenge with EHR-derived data is its source. Because it is aggregated from thousands of disparate systems, it often represents a "lowest common denominator" of data quality.
Internal analysis of raw EHR records reveals significant gaps that most commercial teams don't see until the contract is signed:
Missing Standards: approximately 20-30% of raw records arrive without correct LOINC codes.
Missing Context: Nearly 75% of records lack proper units of measure
Missing Interpretation: Up to 30% of numeric tests fail to include reference ranges or abnormal flags.
For a data science team, this turns a "data asset" into a "data project." Significant resources are burned normalizing and cleaning the feed before any patient identification can begin. In contrast, Direct-Source data ingestion allows for harmonization at the point of entry—correcting codes and units before the data ever reaches the commercial team.
The Latency Trap: The "Rear-View Mirror"
In oncology and rare disease, timing is the only metric that matters. The structural flaw of aggregated EHR data is latency. By the time data is pulled, aggregated, and standardized post-hoc, it often provides a "rear-view mirror" perspective. You are seeing where the patient was weeks or months ago.
Direct-source data operates as a leading indicator. By analyzing clinical evidence—such as abnormal biomarkers or specific protein levels—strategies can identify patients before a confirmed diagnosis code enters the EHR. This shifts the commercial model from reactive (waiting for a claim) to proactive (acting on a signal).
The "Hidden Treater" Phenomenon
Perhaps the most tangible cost of "cheap" data is field force inefficiency. In complex diagnostics, the physician listed on a raw lab record is frequently a Pathologist or Lab Director, not the treating specialist.
Without advanced gap-filling logic to identify the actual treating provider, sales teams often waste valuable territory time visiting pathology labs. Optimized algorithms can now bridge this gap, using historical data to identify the clinician managing the patient. This approach has been shown to increase treating physician fill rates by 70-100%.
The Precision Imperative
Ultimately, the choice of data source dictates the ceiling of your campaign’s success. While EHR-derived data offers breadth, it often lacks the depth and timeliness required for modern therapies.
At Prognos Health, we focus on the latter—delivering enriched, harmonized data that moves faster than the standard of care. Because in precision medicine, the goal isn't just to have data; it's to have the right data, right now. If you'd like to learn more - let's connect: prognoshealth.com/learn-more.