Don’t let clinical blind spots wreck your underwriting risk analysis
- March 30, 2021
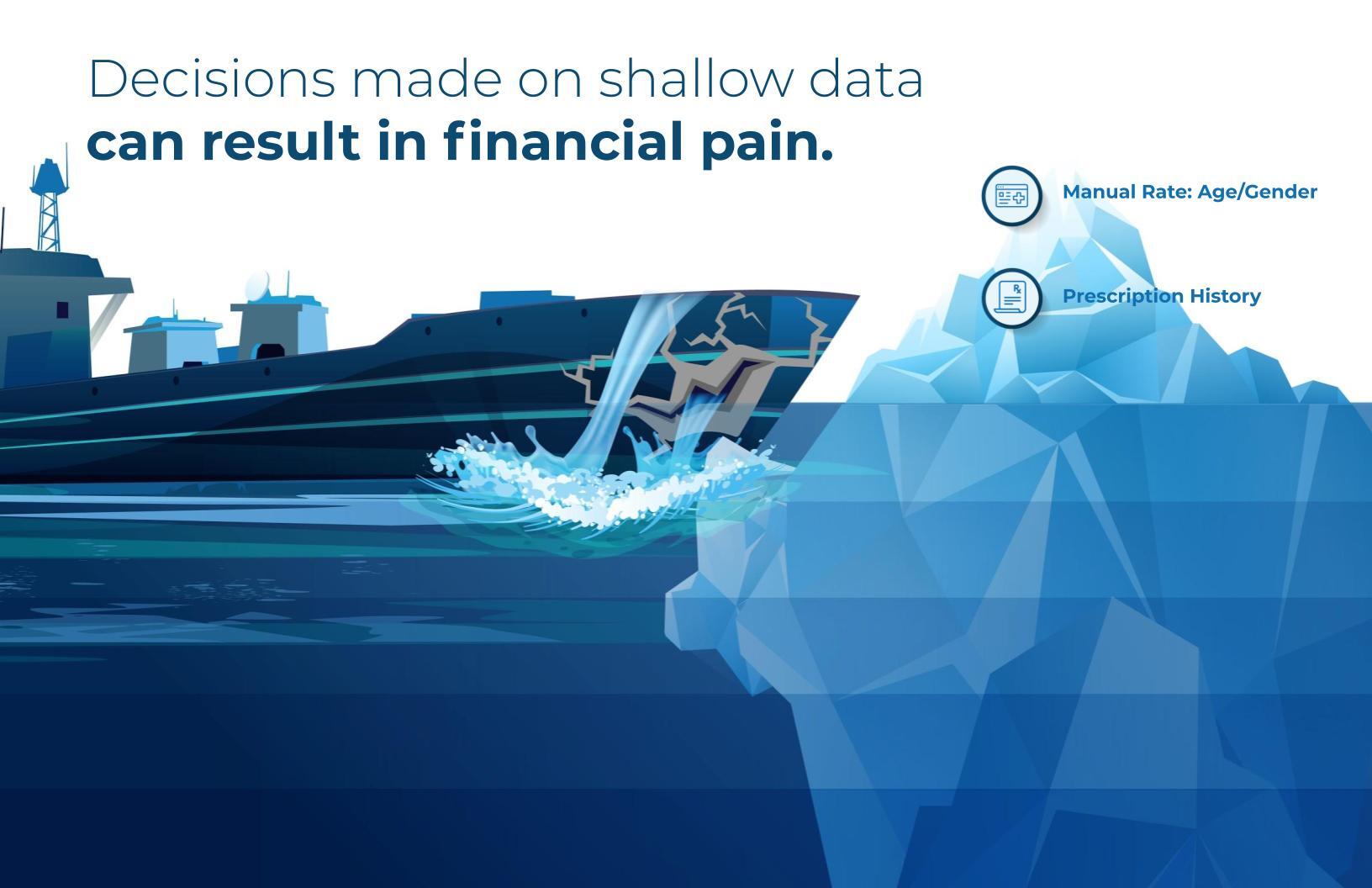
Accurately assigning risk to a group of prospective health plan members is both a science and an art — each part is largely reliant on the quality and comprehensiveness of health data available for that group. This is common knowledge for health insurance Underwriters. It’s also widely known among Underwriters and Actuaries that some frequently used data sources for aggregate risk prediction scores aren’t as complete as they could be. Relying on limited data could paint an incomplete picture of a group’s risk that can open you up to financial losses. What you may not be aware of is that better options for data sources exist that can add a valuable layer of insight to your underwriting risk analysis and predictions, augmenting the gold standard of medical underwriting based upon health questionnaires or prescription histories. This data can protect you from surprises and unenviable financial outcomes.
Prescription data doesn’t tell the whole story
A data source that Underwriters currently depend upon for group risk prediction scoring is made up of deidentified prescription drug histories, in addition to demographic information such as age and gender. While some information can be gleaned from this data, it may not provide a comprehensive picture of the prospective member’s condition.
While prescription history can tell you if a prospective member receives a specific medication, it cannot precisely correlate this information to a medical condition or diagnosis. Furthermore, it cannot tell you if the individual actually used the medication as directed, or at all. For example, a prescription history can tell you if an individual has filled an anti-seizure medication, such as Topamax®, but it cannot tell you if the drug is being used to treat chronic migraines or symptoms of a brain tumor. The underlying diagnosis in this scenario can have a dramatic impact on determining the cost of care for that individual and is material to the overall underwriting decision.
Similarly, prescription information provides little insight into the severity of a prospective member’s disease, nor does it highlight comorbidities. These differences can be glaring. For example, a prescription history can identify phosphate binders, but it cannot tell you if the individual to whom they are prescribed suffers from end stage renal disease or a lesser kidney condition. Disease severity and comorbidities will likely result in much higher medical claims costs.
There is also some latency that is inherent with prescription data. While prescription drug claims are adjudicated relatively quickly, the lag time between initial diagnostic tests, follow-up tests and treatment can result in recently diagnosed conditions being missed during the risk determination and underwriting process.
For large groups with fully credible claims experience, high-risk members can often be adequately absorbed when determining the ongoing costs of care. However, these outliers can have a tremendous negative financial impact when predicting risk for smaller groups. And, with most Payers working with profit margins less than three percent, there’s little room for error or oversight.
Lab data fills gaps, improves underwriting risk analysis and accuracy
The good news is that Underwriters no longer have to rely solely on prescription histories to predict risk. Prognos Health’s Underwriting Risk Predictor adds harmonized laboratory test results to prescription and demographic data to give Underwriters a clearer and deeper understanding of member health and disease severity.
Lab data helps remove much of the ambiguity from the risk determination process. According to the CDC, 70 percent of medical decisions depend on lab results. From a clinical perspective, lab data is the best indicator of disease and treatment, so it’s hard to think of a better information source to predict member risk. Furthermore, lab data provides many additional layers of information than prescription data. Many lab results contain multiple values. The Prognos registry alone contains data on more than 325 million unique patients and includes more than 45 billion distinct lab values. This depth of information provides a comprehensive foundation that equips you for underwriting success.

With lab data, many of the clinical blind spots that exist when relying solely on pharmaceutical data begin to come into focus. The ability to link the presence of multiple blood tests indicating elevated levels of prolactin in the same individual who received that prescription of Topamax suggests a likely treatment for epilepsy which would impact a risk score for that group.
Disease severity can also be better assessed by reviewing lab data. You are able to determine the stage of kidney disease that phosphate binders are being used to treat by examining the blood tests showing the prospective member’s glomerular filtration rate (GFR). Lab results can also provide insight into comorbidities and help you track the progression of a disease and the effectiveness of a particular therapy.
Finally, the information present in lab data is much more timely than that of closed prescription claims. Lab data becomes available as soon as the results are generated and reported, removing latency from the process and providing you with more up-to-date insight into the prospective member’s medical condition.
In short, harmonized lab data integrated with claims encounter data ultimately helps underwriting risk analysis, enabling underwriters to predict a more appropriate rate or premium for a group. This added insight helps protect the Payer, Group, and Reinsurer from potential losses. It can also help you target new groups and bid more accurately and competitively, allowing you to potentially win more deals and grow your block of business.
Learn more about our Underwriting Risk Predictor.